About the London Transformation and Learning Collaborative Critical Care programme
The London Transformation and Learning Collaborative (LTLC) Critical Care programme supports the cross-skilling of the London NHS workforce in response to the Coronavirus pandemic. It aims to broaden the skills base of this workforce to manage existing, and potential future surges in, critical care demand. The programme supports London’s recovery plan by ensuring that:
- training infrastructures can adapt to any future surge and increased critical care capacity
- staff-wellbeing for all colleagues is considered
- opportunities for workforce and training innovations are maximised and continually adapted
Follow updates on Twitter using the hashtag #NHSLTLC or HEE London @NHSHEE_LDN![]()
-
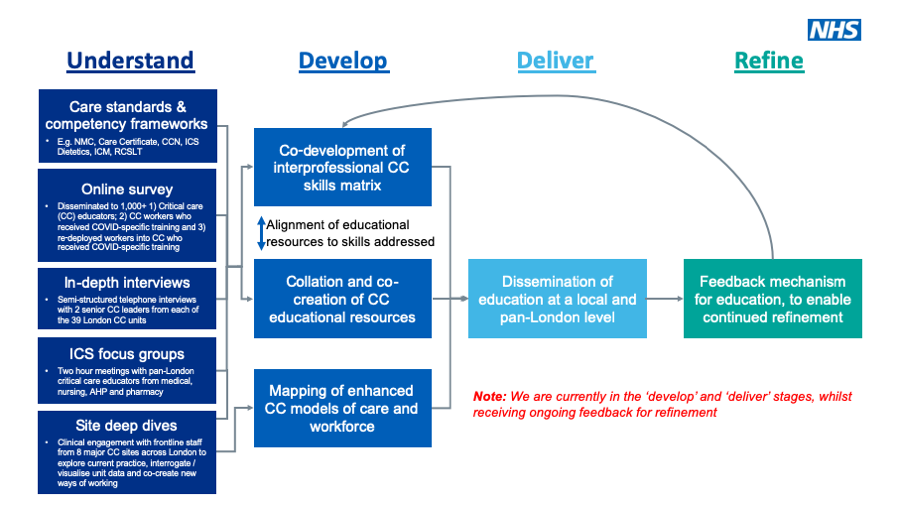
Our approach
The LTLC aims to increase the supply and resilience of London’s critical care workforce through:
- the development of a modular education programme that can be tailored to distinct learner needs
- multi-channel delivery of education to accommodate different skill training requirements and enable wide-spread accessibility
- sharing of practice from critical care units across London (e.g. proformas, job descriptions and reports of positive interventions), that other units may want to consider adopting or adapting
- mapping of optimal critical care workforce models in 8 key surge sites, that will inform their learner needs
- incorporation of a feedback mechanism, to refine and evolve the programme’s educational content over time
The programme is user-led, with both the systems and future learners actively involved in every stage, from development to delivery. We are working with 5 integrated care systems (ICS) in London to ensure we are responsive to different needs across the capital.
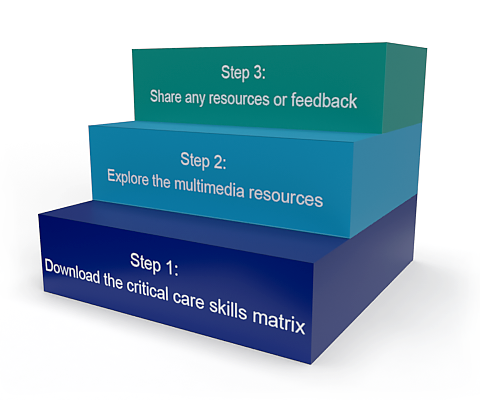
The below chart illustrates the different stages of the programme.
-
Desired outcomes
We have collated educational material for learners and educators that can be tailored to learners’ existing skill level and current, or future, critical care role. These include materials for elearning, face to face teaching, simulation and work-based placements as well as personal development.
For learners, we aim to deliver:
- easy identification of required and desired skills aligned to your current role or expected critical care role
- materials for self-directed learning, resources, and work-based placements to improve confidence and competence working in critical care (including for COVID-19 specifically)
For trainers, we aim to deliver:
- easy identification of required and desired skills aligned to your learners’ current role or expected critical care role
- efficient collation, design and delivery of educational content and train-the-trainer materials to cross-skill the critical care workforce (including for COVID-19 specifically)
For systems, we aim:
- to build the capability of the London NHS workforce capability to enable it to operate at a new, increased critical care capacity (our primary goal)
- to demonstrate a new agile model for developing and delivering education rapidly in response to changing national healthcare requirements, in collaboration with existing regional systems (our secondary goal)
COVID-19 Surge 2021 – Rapid Access Resources
To support NHS staff being deployed for the Coronavirus response, the LTLC have collated some key resources to help individuals, educators and systems prepare. We recognise staff are very busy; so these resources are purposely designed to be short and read/watched on the move or the ward.
How to use this programme and microsite
Learners interested in resources to educate themselves should download How to use this programme for Learners (PDF, 153KB) for detailed instructions on how to use this programme. Further information is available below.
Trainers interested in resources to train others should download How to use this programme for Trainers (PDF, 121KB) for detailed instructions on how to use this programme. Further information is available below. Those interested in content to inform critical care units or system operations should download How to use this programme for Critical Care Unit or System (PDF, 119KB) for detailed instructions on how to use this programme. Further information is available below.
Step One: Interprofessional skills matrix
We have developed a skills matrix that maps the most useful educational content to the skills they address, by professional group or role within critical care, and for learners and trainers. The content is matched against NMC, GMC, HCPC, NCFRN CC3N and CoBaTrICE professional competencies to aid presentation for revalidation and appraisal.
Download the ![]() (Microsoft Excel, 194KB)
(Microsoft Excel, 194KB)
The skills matrix is under active revision, so please regularly check this document for the latest version. Latest additions include:
- Pharmacy resources (critical care specific)
Current updates in progress include:
- Redeployed staff resources
The searchable equipment training matrix is available under ‘Generic Skills (includes Safety, Communication, Wellbeing, Human factors)’ either below, or via the elfh Hub.
-
About the skills matrix
About the skills matrix
The matrix includes recommended skills for the following posts:
- ICU Generic Skills: for all staff members deployed to work in ICU. These are the basic requirements.
- COVID-19 Generic Skills: for all staff members working within a COVID-19 area.
- NRSS (Non-Registered Support Staff): for all staff who are not registered under a professional body.
- RSC (Registered Support Clinician): for all staff who are registered under a professional body (e.g. NMC, GMC, HCPC). They may be redeployed to critical care areas during surge or caring for patients on wards who are more unwell than usual (deteriorating/ICU step down). These learning outcomes have all been mapped where possible to the CC3N Step 1 competencies (National Clinical Framework for Registered Nurses (NCFRN) for Adult Critical Care Nurses Critical Care Networks National Nurse leads (CC3N) Step 1 competencies)
- PT (Physiotherapist): for physiotherapists with minimal or no previous ICU experience (skills matrix in early stages of development – significant revision required)
- OT (Occupational therapist): for occupational therapists with minimal or no previous ICU experience (skills matrix in early stages development – significant revision required)
- SLT (Speech and language therapists): for speech and language therapists with minimal or no previous ICU experience (skills matrix in early stages of development – significant revision required)
- Dieticians: for dieticians with minimal or no previous ICU experience (skills matrix in early stages of development – significant revision required)
Note: AHP roles may vary depending on local workforce planning. The skill matrix focusses on cross-skilling non-critical care specialist AHPs to be competent in working within ICU, undertaking tasks that will allow experience critical care AHPs and other team members to deliver more complex tasks requiring more extensive training.
- HCS (Healthcare Scientists): skills matrix in early stages of development – significant revision required
- Pharmacy (Pharmacists): not yet available
- Surge Doctor: 1. doctors who have had minimal (less than 3 months) or no previous ICU experience OR 2. non critical care doctors who have had more than 9 months of critical care experience. They may be redeployed to critical care areas during surge or caring for patients on wards who are more unwell than usual (deteriorating/ICU step down). These learning outcomes have all been mapped to help learners track their self-development to their own training and revalidation needs as appropriate. Curricula mapped to are:
– Competency Based Training in Intensive Care Medicine in Europe competencies (CoBaTRice)
– Faculty of Intensive Care Medicine (FICM) Core and Common competencies (which map against ACCS, CAT & CMT competencies)
– GMC Good Medical Practice (GMP)
The skills matrix has been created to assist with cross skilling staff in preparation for ICU bed expansion. The skills and learning objectives are taken from national frameworks for individual professional bodies. If a skill falls under a particular competency framework, this has been mapped on the matrix. This is not a prescription of the skills to be undertaken by each role, they are recommendations as to what essential and priority skills are deemed to be necessary to allow flexibility within an ICU team but with precedence on safe patient management. It is not designed to limit a professional scope. The intention is to cover the key interventions and therapies available within intensive care; any additional specialised intervention and therapies may be beyond the scope of this matrix. The skills and roles will require adaptation to local workforce and care remodelling. The skills are suggestions as to what we feel should be delivered with the delivery being undertaken by local teams.
Step Two (for learners): Educational resources
The current educational resources available for learners can be found below. These have been mapped to the skills matrix by professional grouping. We are still in the resource collation and co-creation phase and would appreciate you sharing any relevant resources (please see the below ‘How to give your feedback’ section).
Generic Skills (includes safety, communication, wellbeing, human factors) and COVID-19 Generic Skills are the basic skills required by all healthcare professionals working in the critical care and/or COVID-19 environments. Additional skills and resources are described in the individual professional grouping sections.
-
Generic Skills (includes Safety, Communication, Wellbeing, Human Factors)
For all staff members deployed to work in ICU. These are the basic requirements.
Safety
- Bedside patient safety checks
- Infection prevention & control
- Cardiac arrest
- Debriefing
- Local induction
Communication
Documentation
Moving and Handling
Professional Development
Human factors
- Teamwork followership
- Teamwork: MDT
- Teamwork leadership
- Human factors: handover
- Human factors: decision making
- Human factors: assertiveness
- Human factors: escalation
- Human factors: risk management
- Human factors: stress and resilience
Wellbeing
ICU Generic Resources
Equipment Matrix
To support you finding approved training and support resources for equipment, we have created an Equipment Support Matrix. The ‘Dashboard’ tab allows the user to select from a drop down list the type of equipment e.g. ventilator, then the manufacturer and finally the model. Once selections from all 3 drop down lists have been made the links will update and direct the user to the elearning for Health resources available.
Please note, while these are the most accessible guides available, some may not be from manufacturers, and all should be reviewed by site practice development/education/technical/scientist teams to ensure that they are appropriate for local practices.
Download the
 (Microsoft Excel, 92KB)
(Microsoft Excel, 92KB)Alternatively, you can access our mobile friendly web app.
The equipment matrix is under continuous development, so your input is highly valued. Please contact LTLC at ltlc@hee.nhs.uk with any feedback, suggestion or request, quoting ‘equipment matrix’ in the subject line. Thank you very much in advance.
-
COVID-19 Generic Skills
For all staff members working within a COVID-19 area.
Safety
Communication
COVID-19 Generic Resources
-
RSC (Registered Support Clinician) – staff who are registered under a professional body (e.g. NMC, GMC, HCPC)
An RSC may be:
- a junior ICU nurse who has not yet achieved their step 1 competencies in the National Competency Framework,
- a registered nurse, who works outside of ICU or
- a registered (non-nursing) health care professional.
The RSC may be redeployed to critical care areas during surge or caring for patients on wards who are more unwell than usual (deteriorating/ICU step down). These learning outcomes have all been mapped where possible to the CC3N Step 1 competencies (National Clinical Framework for Registered Nurses (NCFRN) for Adult Critical Care Nurses Critical Care Networks National Nurse leads (CC3N) Step 1 competencies).
To accompany these resources a “skills passport” has been developed to highlight the most important skills for the Registered Support Clinician to hold before starting work on a critical care unit (as identified by senior critical care nurses and educators across London). This skills passport can be accessed digitally for NHS London staff or a downloadable Microsoft Word version (40KB) and both contain:
- An introduction to the passport
- Passport Assessment tool for RSC Staff
- Statement of Competence – to be completed by RSC and supervisor
- Links to elfh resources identified to help achieve RSC status if needed
Safety
Airway
- Endotracheal tube care
- Mouth care (for intubated and non-intubated patients)
- Mouth care (for intubated patients)
- Tracheostomy care
- Airway essential
Breathing
- Respiratory physiology
- Ventilator management
- Chest drain management
- Non-invasive ventilation
- Weaning from ventilation
- Additional therapy
- Oxygen therapy – step down specific
Circulation
- Arterial line management
- Central venous catheter management (inc. care bundle)
- Fluid prescription
- Fluid administration
- Fluid balance
- 12 lead ECG
GI
- Insertion of NGT in sedated/unsedated/ventilated/non ventilated patient
- Dysphagia and oral feeding
- Administration and troubleshooting of NG feed
Neurology
Medication
- Administration of drugs nasogastrically – Content required: please see section below on How to give your feedback and share resources
- Administration of IV therapy
- IV drugs – preparation / administration or prescription – Content required: please see section below on How to give your feedback and share resources
- IV infusions – preparation / administration / management of infusion device or prescription – Content required: please see section below on How to give your feedback and share resources
- VTE thromboprophylaxis
- GI prophylaxis
- Glycaemic control
Assessment, Monitoring and Interpretation
- Taking and recording of vital signs
- Systematic nursing patient assessment
- Observation chart step down
- Electrolyte abnormalities
- Waveform recognition and escalation – Content required: please see section below on How to give your feedback and share resources
- Renal replacement therapy
- Renal physiology – Content required: please see section below on How to give your feedback and share resources
Equipment
- Ventilator management
- Waveform recognition and escalation
- IV infusions – preparation / administration / management of infusion device or prescription
Bedside and patient hygiene
EOL care
Rehabilitation
Transfer
-
NRSS (Non Registered Support Staff) – staff who are not registered under a professional body
An NRSS may be:
- a Health Care Support Worker or
- a non-registered member of staff specifically recruited to ICU in this role
- healthcare students who may wish to work on Critical Care Units during the surge as bank staff
The NRSS may be redeployed to critical care areas during surge or caring for patients on wards who are more unwell than usual (deteriorating/ICU step down).
To accompany these resources a “skills passport” has been developed to highlight the most important skills for the Non-Registered Support Staff member to hold before starting work on a critical care unit (as identified by senior critical care nurses and educators across London). This skills passport document (PDF, 170KB) is a downloadable PDF which contains:
- An introduction to the passport
- Passport Assessment tool for RSC Staff
- Statement of Competence – to be completed by NRSS and supervisor
- Links to elfh resources identified to help achieve NRSS status if needed
Safety
Airway
- Mouth care (for intubated and non-intubated patients)
- Mouth care (for intubated patients) – Content required: please see section below on How to give your feedback and share resources
- Airway essential
Breathing
Circulation
GI
Neurology
Assessment, Monitoring and Interpretation
- Taking and recording of vital signs
- Systematic nursing patient assessment
- Observation chart ICU
- Observation chart step down
- Renal replacement therapy
Bedside and patient hygiene
EOL care
Rehabilitation
Admission
Transfer
-
PT (Physiotherapist)
For physiotherapists with minimal or no previous ICU experience.
Safety
Airway
- Endrotracheal tube care
- Mouth care (for intubated and non-intubated patients)
- Tracheostomy care
- Tracheostomy weaning
- Airway essential
Breathing
- Respiratory physiology
- Ventilator management
- CXR interpretation
- Non-invasive ventilation
- Chest drain management
- Weaning from ventilation
- Additional therapy
- Oxygen therapy – step down specific
Circulation
- Arterial line management
- Central venous catheter management (inc. care bundle)
- Fluid prescription
- 12 lead ECG
GI
Neurology
Medication
Assessment, Monitoring and Interpretation
- Taking and recording of vital signs
- Systematic patient assessment
- Observation chart (ICU)
- Arterial blood gas interpretation
- Respiratory assessment
Equipment
- Ventilator management
- IV infusions – preparation / administration / management of infusion device or prescription
Bedside and patient hygiene
EOL care
Rehabilitation
Moving and Handling
-
OT (Occupational therapists)
For occupational therapists with minimal or no previous ICU experience.
Safety
Airway
- Intubation and/or reintubation
- Endotracheal tube care
- In-line suctioning
- Mouth care (for intubated and non-intubated patients)
- Tracheostomy care
- Airway essential
Breathing
- Ventilator management
- Chest drain management
- Non-invasive ventilation
- Weaning from ventilation
- Oxygen therapy – step down specific
Circulation
GI
Neurology
Assessment, Monitoring and Interpretation
Equipment
- Ventilator management
- IV infusions – preparation / administration / management of infusion device or prescription
Rehabilitation
Moving and Handling
Bedside and patient hygiene
-
SLT (Speech and language therapists)
For speech and language therapists with minimal or no previous ICU experience.
Safety
Airway
- Mouth care (for intubated and non-intubated patients)
- Tracheostomy care
- Tracheostomy weaning
- Airway essential
Breathing
- Respiratory physiology
- Ventilator management
- Non-invasive ventilation
- Oxygen therapy – step down specific
Circulation
GI
- Insertion of NGT in sedated/unsedated/ventilated/non ventilated patient
- Dysphagia and oral feeding
- Administration and troubleshooting of NG feed
Neurology
Equipment
- Ventilator management
- IV infusions – preparation / administration / management of infusion device or prescription
Bedside and patient hygiene
EOL care
Rehabilitation
-
ODP (Operating Department Practitioner)
For Operating Department practitioners with minimal or no ICU experience.
Safety
Airway
- Endotracheal tube care
- Mouth care (for intubated and non-intubated patients)
- Mouth care (for intubated patients)
- Trachesotomy care
- Airway essential
Breathing
- Respiratory physiology
- Ventilator management
- Non-invasive ventilation
- Additional therapy
- Oxygen therapy – step down specific
Circulation
- Arterial line management
- Central venous catheter management (inc. care bundle)
- Fluid prescription
- Fluid administration
- Fluid balance
- 12 lead ECG
GI
- Insertion of NGT in sedated/unsedated/ventilated/non ventilated patient
- Dyspagia and oral feeding
- Administration and troubleshooting of NG feed
Neurology
Medication
- Administration of IV therapy
- IV drugs – preparation / administration or prescription
- IV infusions – preparation / administration / management of infusion device or prescription
- VTE thromboprophylaxis
- GI prophylaxis
- Glycaemic control
Assessment, Monitoring and Interpretation
- Taking and recording of vital signs
- Systematic nursing patient assessment
- Electrolyte abnormalities
- Renal replacement therapy
Equipment
- Ventilator management
- Waveform recognition and escalation
- IV infusions – preparation / administration / management of infusion device or prescription
Bedside and patient hygiene
EOL care
Rehabilitation
Transfer
-
Dieticians
For dieticians with minimal or no previous ICU experience.
Safety
Airway
Breathing
Circulation
- Arterial line management
- Central venous catheter management (inc. care bundle) (in development)
- Fluid balance
GI
- Insertion of NGT in sedated/unsedated/ventilated/non ventilated patient
- Administration & troubleshooting of NG feed
Neurology
Medication
Assessment, Monitoring and Interpretation
Equipment
- Ventilator management
- IV infusions – preparation / administration / management of infusion device or prescription
EOL care
Rehabilitation
-
HCS (Healthcare Scientists)
Healthcare scientist (HCS) as a title encompasses a very varied workforce who work in departments from pathology to radiotherapy, through to sleep studies and data analytics. In response to the first COVID surge HCS performed many different roles and had a whole host of responsibilities outside of BAU.
HCS were redeployed as ICU tech support, clinical engineering support, bedside buddies and floating clinical team (at NHS London Nightingale Hospital).
HCS Surge Roles (PDF, 882KB) offers a brief introduction to how HCS could add value in a surge situation
Medical Equipment safety and QA HCS role (PDF, 547KB) provide some details regarding this final role.
Most trusts have a lead HCS who can help identify HCS staff and aid in establishing where their skills could be best utilised.
Equipment
Safety
-
Pharmacy (Pharmacists)
Safety
Airway
Breathing
Circulation
- Arterial line management
- Central venous catheter management (inc. care bundle)
- Intravenous vasocative drugs
- Fluid administration
- Fluid balance
GI
Neurology
- Monitoring, managing and weaning sedation
- Glasgow coma score
- Pain management
- Delirium recognition and management
- RASS & CPOT pain scores
Medication
- Respiratory system
- Central nervous system
- Infections
- Endocrine system
- Eye
- Anaesthesia
- Renal impairment
- Parenteral therapy
- Toxicology
- Haemostasis and thrombosis
- Medicine supply
- Medicines reconciliation and de-prescribing
Palliative and EOL care
Transfer
-
Surge Doctor
1. doctors who have had minimal (less than 3 months) or no previous ICU experience OR 2. non critical care doctors who have had more than 9 months of critical care experience. They may be redeployed to critical care areas during surge or caring for patients on wards who are more unwell than usual (deteriorating/ICU step down). These learning outcomes have all been mapped to help learners track their self-development to their own training and revalidation needs as appropriate. Curricula mapped to are:
– Competency Based Training in Intensive Care Medicine in Europe competencies (CoBaTRice)
– Faculty of Intensive Care Medicine (FICM) Core and Common competencies (which map against ACCS, CAT & CMT competencies)
– GMC Good Medical Practice (GMP)Safety
Airway
- Intubation and/or reintubation
- Endrotracheal tube care
- In-line suctioning
- Tracheostomy care
- Airway essential
Breathing
- Chest drain insertion (Seldinger and tube thoracostomy)
- Non-invasive ventilation
- Ventilator management
- Weaning from ventilation
- CXR interpretation (expected to be prior knowledge for all doctors)
- Chest drain management
Circulation
- 12 lead ECG
- Arterial line insertion
- Arterial line management
- Central venous catheter management (inc. care bundle)
- Fluid prescription
- Intravenous vasoactive drugs
- Fluid balance
GI
Neurology
- Monitoring, managing and weaning sedation
- Glasgow coma score
- AVPU
- Delirium recognition and management
- Pain assessment in awake patients
- RASS & CPOT pain scores
Medication
- Antimicrobials
- IV infusions – preparation / administration / management of infusion device or prescription
- VTE thromboprophylaxis
- GI prophylaxis
Assessment, Monitoring and Interpretation
- Taking and recording of vital signs
- A to E assessment
- Critical care patients – full assessment
- Hypoglycaemia and management
- Electrolyte abnormalities
- Waveform recognition and escalation
- Arterial blood gas interpretation
- Renal replacement therapy
Moving and Handling
Bedside and patient hygiene
EOL care
- Completing respect forms/DNAR
- End of life prescription
- Last offices
- Symptom control
- End of life care
- Chaplaincy
Documentation
Transfer
Redeployment
This Surge Doctor Redeployment Suggestions document provides suggestions compiled by the LTLC for supporting the training and well-being doctors being redeployed into critical care. This method allows opportunities for ongoing training and to give appropriate support to critical care as and when the surge need arises. It is up to individual Trusts to determine the exact arrangements that best support patient care. Any redeployments will require the specific approval of the Postgraduate Dean (or nominated deputy).
Step Two (for trainers): Educational resources
The current educational resources and train-the-trainer materials can be found below. These have been mapped to the skills matrix by professional grouping. We are still in the resource collation and co-creation phase and would appreciate you sharing any relevant resources (please see the below ‘How to give your feedback’ section).
-
Programme Outlines / Timetables
- Red training plan from NHS Nightingale London Education team – suitable for NRSS (2-day)
- Amber training plan from NHS Nightingale London Education team – suitable for RSC (2-day)
- COVID Preparation Course, Level 2 & Level 3 Patient Care – 2 Day Programme from Epsom & St. Helier NHS Trust – suitable for RSCs.
- COVID-19 redeployed staff Critical Care training programme from Barts Health NHS Trust, 2 day programme – suitable for redeployed staff as refresher training or surge doctors.
- Training programme for redeployed staff in Critical Care: COVID 19 from Homerton University Hospital NHS Foundation Trust – facilitator handbook for 1 day course with online lecture preparation (links included); suitable for RSCs and NRSS.
- NWL Surge Tracheostomy Training from North West London Safer Tracheostomy Care Collaborative – comprehensive training programme including lectures and competency booklets.
- ICU Cross-Skilling Course for Redeployed Staff
- COVID-19 On the Wards: Remote video debriefing course
Content required: please see section below on How to give your feedback and share resources.
-
Clinical Care
Safety (from RSC/NRSS e.g. teaching material for bedspace safety checks)
- Levels of care
- Bed space preparation (in development)
- Bedside safety checks
- Bedside safety checks/equipment (in development)
- Cardiac arrest
- Cardiac arrest in the COVID patient
- Debriefing
- End of shift debriefing (leading)
- Infection prevention & control
- Local Induction
- Patient safety (in development)
- PPE donning & doffing
- Catastrophic (mass) oxygen failure
- Risk management (in development)
Airway
- Airway essential
- Endotracheal tube care
- In-line suctioning
- Intubation and/or reintubation
- Mouth care (for intubated and non-intubated patients)
- Mouth care (for intubated patients)
- Tracheostomy care
- Tracheostomy weaning (in development)
Breathing
- Non-invasive ventilation
- Assessment
- Respiratory physiology
- Ventilator management
- Chest drain management
- Additional therapy
- Oxygen therapy – Step down specific
- Chest drain insertion (Seldinger and tube thoracostomy) (in development)
- Weaning from ventilation
- CXR interpretation
Circulation
- 12 lead ECG (in development)
- Arterial line insertion (in development)
- Arterial line management
- Central venous catheter management (inc. care bundle)
- Fluid administration
- Fluid balance
- Fluid prescription (in development)
- Insertion of central lines (in development)
- Intravenous vasoactive drugs
- Venepuncture and Insertion of peripheral lines (in development)
Gastrointestinal (GI)
- Dysphagia and oral feeding (in development)
- Administration and troubleshooting of NG feed
- Dietetic Care Plan (in development)
- Enteral and parenteral feeding (in development)
- Estimating targets (in development)
- GI function (in development)
- Insertion of NGT in sedated/unsedated/ventilated/non ventilated patient
- Metabolic response (in development)
- NG (in development)
- NG feed / medications (in development)
- Nutritional diagnosis (in development)
- Nutritional intervention (in development)
- Nutritional screening (in development)
- Refeeding (in development)
- GI prohylaxis
Neurology
- AVPU (in development)
- Delirium recognition and management
- Glasgow coma score
- Monitoring, managing and weaning sedation
- Pain management
- Pain assessment in awake patients (in development)
- RASS & CPOT pain scores
Medication
- Administration of drugs nasogastrically
- Administration of IV therapy
- Antimicrobials
- Drug chart & prescription protocols
- GI prophylaxis
- Glycaemic control (in development)
- Infections
- IV drugs – preparation / administration or prescription
- IV infusions – preparation / administration / management of infusion device or prescription
- Recognition of common medications (in development)
- VTE thromboprophylaxis
Assessment, Monitoring and Interpretation
- A to E assessment
- Arterial blood gas interpretation
- Critical Care patients – full assessment
- Electrolyte abnormalities
- Hypoglycaemia and management
- IV infusions – preparation / administration / management of infusion device or prescription (in development)
- Observation chart (ICU)
- Observation chart step down
- Outcome measures (in development)
- Renal physiology (in development)
- Renal replacement therapy (in development)
- Respiratory assessment (in development)
- Systematic nursing patient assessment
- Taking and recording of vital signs
- Waveform recognition and escalation (in development)
Equipment
- Optimisation of medical device effectiveness and efficiency (in development)
- Planned maintenance and repairs to devices (in development)
- Rehabilitation equipment (in development)
- Risk management and governance (in development)
- Ventilation
- Ventilator management (in development)
- Waveform recognition and escalation
Bedside and Patient Hygiene
- Bedside cleaning (in development)
- Eye care
- Personal care
- Skin care
- Pressure care
- Stocking/Transport of samples and collection (in development)
- Urinary catheter care
- Urinary catheterisation
- Washing & personal hygiene
Moving and Handling
- Moving and handling patients
- ADL support
- Falls prevention
- Proning
- Rehabilitation (in development)
Admission
- Admission (in development)
Documentation
- Local IT training
- Transfer and Discharge (in development)
Transfer
- Intrahospital (in development)
- Intrahospital / Interhospital (in development)
-
Rehabilitation and End of Life Care
Rehabilitation
End of Life (EOL) Care
- Chaplaincy
- Communication with family
- Completing Respect forms/DNAR (in development)
- End of life care (in development)
- End of life care plan (in development)
- End of life prescription (in development)
- Last offices
- Symptom control (in development)
-
Professional Development, Human Factors and Communication
Professional Development
- Clinical governance (in development)
- Clinical practice (in development)
- Human factors: assertiveness
- Human factors: decision making
- Human factors: escalation
- Human factors: graded assertiveness
- Human factors: handover
- Human Factors: leadership (in development)
- Human factors: risk management
- Human factors: stress and resilience
- Human factors: teamwork
- Professional practice
- Professionalism
- Research, Development and Innovation (in development)
- Teamwork: followership
- Teamwork: leadership
- Teamwork: MDT
Communication
-
Wellbeing
-
Train the Trainer
-
Simulation
Step Two (for Critical Care Units or Systems): Great operational practices
The LTLC programme includes networking across the whole of London and learning from the great practices in each of the Critical Care Units.
Please see below the current resources available which have been shared through this pan-London network as examples of great practices. Though they may be site specific, we hope that by sharing them here, other units can learn and adapt these to their own needs, and share their own great practices in return.
We are still in the resource collation and co-creation phase, therefore we would appreciate you sharing any relevant resources (please see below the ‘How to give your feedback’ section). We also are a continuously learning ourselves so all feedback, ideas and comments gratefully received – both constructive and positive!
-
A Toolkit for rapid cross-skilling, supporting safe redeployment
A Toolkit for rapid cross-skilling, supporting safe redeployment
As we are met with immense pressures and the need to redeploy staff safely across healthcare settings, the LTLC have created a toolkit, compiling guidance and resources to support interprofessional cross-skilling during rapid redeployment of the workforce.
The attached toolkit (PDF, 1448KB) provides guidance on the resources available on the LTLC website which should be used in conjunction with updated national guidance for workforce management published on 10 December 2020, Advice on Acute Sector Workforce Models During Covid-19 (PDF, 686KB). The toolkit is packed with hyperlinks and QR codes to take users direct to the core content.
Download, share via social media or print and post in your department / coffee room / changing room this interactive PDF on “How to access the LTLC Resources for Redeployment (PDF, 191KB).”
-
Just-in-time training for Deployed Staff
Just-in-time training for Deployed Staff
 These Just-in-time training packages for deployed staff collates COVID response essential skills for staff being (re)deployed, with rapid access links to help them cover the essential skills that may be needed by anyone working outside their normal role in surge. These essential skills have been divided into steps, from how to access COVID specific self-directed learning through to completing a skills passport.
These Just-in-time training packages for deployed staff collates COVID response essential skills for staff being (re)deployed, with rapid access links to help them cover the essential skills that may be needed by anyone working outside their normal role in surge. These essential skills have been divided into steps, from how to access COVID specific self-directed learning through to completing a skills passport.Just-in-time training fundamentals (PDF, 403KB)
Doctor redeployment Just-in-time training (PDF, 441KB)
-
RSC / NRSS Task Allocation for ‘Pod’ Structure and Passports
RSC / NRSS Task Allocation for ‘Pod’ Structure and Passports
During surge, nursing care can be delivered in a ‘Pod’ structure. The ICU Nurse ‘leads’ the Pod, and identifies the skill set of any team members who may be:
- Registered Support Clinicians (RSC) or
- Non-Registered Support Staff (NRSS)
This Guide for allocation in surge model of critical care nursing (PDF, 179KB) sets out a suggested way that tasks can be allocated within the pod as a guidance for any trusts new to this style of nursing. The critical care nurse can allocate, and supervise where required, tasks according to this. It is imperative that critical care nursing staff are still supported by their seniors and given opportunities to reflect on and develop their leadership skill in order to help support their wellbeing.
Resources:
RSC Digital passport – currently for London NHS staff
RSC Skills Passport (Microsoft Word document, 40KB)
NRSS Skills Passport (PDF, 170KB) -
Staff Wellbeing Bundle
Staff Wellbeing Bundle
Bundle of resources developed at Epsom & St Helier Trust aimed at preserving and enhancing staff wellbeing:
- wellbeing support booklet (detailed resources)
- staff wellbeing pamphlet
- spiritual support booklet (patients and staff)
- specialist Filipino support service
- mental wellbeing while staying at home
- health and wellbeing programme example
- culturally diverse virtual staff common room flyer
Select this link to access this resource on the elfh Hub.
-
SBAR ABCDE Critical Care Handover Tool
SBAR ABCDE Critical Care Handover Tool
Structured handover document using SBAR (situation, background, assessment, recommendations) & ABCDE formats combined to allow a structured focused handover of critical care patients.
Introduced as a quality improvement tool, particularly in the context of stretched nursing rations and less experienced staff, this guide has reduced the time taken to handover patients, with an increase in staff satisfaction and no deterioration in the quality of handover.
Select this link to access this resource on the elfh Hub.
-
Paediatric critical care nurses cross-skilling documents
Paediatric critical care nurses cross-skilling documents
Skills Matrix addition
A column has been added to the RSC tab of the Skills Matrix called “Redeploying paediatric staff areas to update”. This highlights the learning outcomes that staff who redeployed from paediatrics to adult critical care in surge 1 felt they needed to revise to feel confident in the adult environment. Each of these is mapped to resources that are readily available through the LTLC elfh hub.In addition, as for all staff redeploying, there are key skills covered in both the ‘ICU Generic Skills’ tab and the ‘Covid-19 Generic Skills’ tab such as ‘proning’ and ‘manual handling’ videos and patient safety resources.
Additional resources have been provided by colleagues from across London:
- Report on supported redeployment of PICU staff to general paediatric ward (Microsoft Word document, 13KB) (GOSH to the Whittington Hospital)
- 17-page guidance document for PICU staff being redeployed to ACC in surge 1 (PDF, 941 KB) (North Thames Paediatric Network)
- Evaluation paper Burnett et al. (2020) (PDF, 383KB) sharing the experiences of 25 redeployed PICU staff during surge 1
-
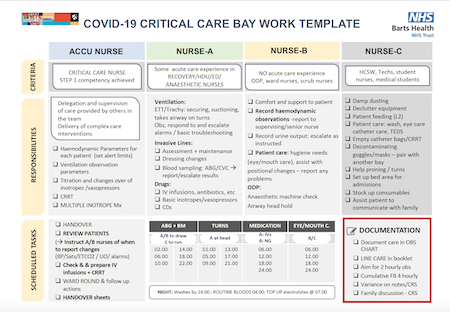
Bay Template
Bay Template
Bay Template
COVID-19 Critical Care Bay Work Template – example of critical care trained, registered support clinicians and non-registered support staff criteria, responsibilities, & tasks working as a small team caring for patients; includes example 24hr work plan.
Select this link to access this resource on the elfh Hub.
-
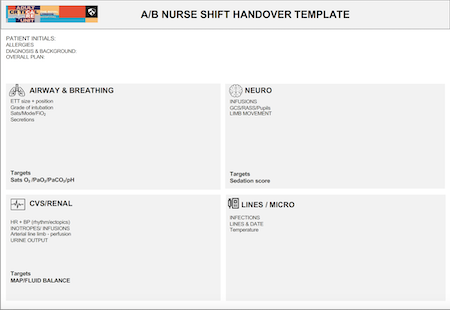
Nurse Shift Handover Document
Nurse Shift Handover Document
Nurse Shift Handover Document
Nursing shift handover document highlighting important point to handover to the next shift, red flag alerts as prompts for emergency escalation, and summaries of all patients in the bay. Hourly slots in which key events can be recorded if required e.g. ‘proned’, ‘transfer to CT scan’.
Select this link to access this resource on the elfh Hub.
-
COVID-19 Critical Care Plan - A Resilient Approach
COVID-19 Critical Care Plan - A Resilient Approach
COVID-19 Critical Care Plan – A Resilient Approach: Outline of the development of resilient critical care approach to future COVID-19 surges or other surges in critical care demand, covering roles (including Critical care Nurse, Registered Support Clinician, and support staff), allocation & escalation, and an RSC Basic ICU Skills passport.
Select this link to access this resource on the elfh Hub.
-
Daily shift planners for NRSS staff on Critical Care
Daily shift planners for NRSS staff on Critical Care
Daily shift planners for NRSS staff on Critical Care – Shift planning resource for both unit-facing and patient-facing roles, allowing the allocation of a structured plan for the day, and suggestions for patient, bay/pod, and unit level task suggestions.
Select this link to access this resource on the elfh Hub.
-
COVID-19 Critical Care Made Easy Guide
COVID-19 Critical Care Made Easy Guide
A brief introduction to the management of the COVID-19 patient on critical care, covering mechanical ventilation, monitoring & imaging, proning, vasopressors & inotropes, renal replacement and acute kidney injury (AKI).
Select this link to access this resource on the elfh Hub.
Step Two: Field Hospital Resources
-
NHS Nightingale London Educators Resources
The core aim of the NHS Nightingale London Education and Training curriculum was to develop staff who were confident and able to practice safely in their allocated roles within the NHS Nightingale Field Hospital at The ExCel Centre. Between March and May 2020 over 2,700 learners were trained face-to-face and a further 1,000 participated in on-line training.
Learning was all delivered interprofessionally and was were organised into four broad programmes as outlined below and has well-being threaded through. All of these programmes also had corporate and local clinical induction sessions. It is important not to forget the importance of Local Clinical Induction for staff new to a Critical Care Unit.
(further information available in the ‘Overview Documents‘ section)
Green education and training for those working in an ICU role already.
Amber education and training for registered healthcare professionals who will be working in a critical care role that is different to their current role and require some additional critical care training to enable them to do the job. Ideal for RSC training.
Red education and training for those who will be working in a critical care unit in a role that is significantly different to their current practice: They may not have any health or care experience. These roles do not have direct patient responsibility but will be part of care teams such as Washing, Turning etc. Ideal for NRSS training.
Purple education and training for those who will be undertaking a specialist role in the critical care unit that is the same as their current NHS role.
Curriculum Components Red training Amber training Green training Purple training Safety Critical Training Corporate and Local Clinical Induction PPE Communication Wellbeing (PsychPPE) Compassionate Care Documentation Pharmacy skills Safety Critical Clinical Skills COVID Cardiac Arrest (and prone pt) Airway Breathing Circulation Fluids In Fluids Out Patient positioning, moving and handling Consolidation of Learning Full Immersion Clinical Simulation Day Zero
The underlying principles of Day Zero are to alleviate anxiety and to deliver learning needs not met within induction. The aims when used at NHS Nightingale London were:
- To orientate staff to the hospital site, ward space, equipment and hospital layout
- To focus on patient safety and prepare people to step onto a critical care unit on a “day one”
- To identify outstanding learning objectives for new starters at NHS Nightingale London and meet them or signpost to where they can be met
- To alleviate anxieties prior ahead of clinical work the Nightingale London
- To reinforce messages around culture and well-being
Posters
These posters were developed to support the training of staff for NHS Nightingale London and to be used in the clinical areas to remind staff of key information about communication tools including SBAR, CUSS, Closed-loop communication and Hand signals for non-verbal communication.
Simulation Scenarios
These scenarios were written to support the face-to-face training within the London Nightingale Education team.
They are designed for a range of participants from those with no healthcare experience (red) through to pre-existing ICU staff (green) tackling more complex issues.
-
NHS Nightingale Yorkshire & Humber Educators resources
The core aim of the NHS Nightingale Yorkshire & Humber Education and Training curriculum was to develop staff who were confident and able to practice safely in their allocated roles within the NHS Nightingale Field Hospital at The Harrogate Convention Centre.
Learning was all delivered interprofessionally and organised into three broad programmes as outlined below. All of these programmes had corporate and local clinical induction sessions. It is important not to forget the importance of Local Clinical Induction for staff new to a Critical Care Unit.
(further information available in the ‘Overview Documents‘ section)
Blue education and training for those working in an ICU role already.
Yellow education and training for registered healthcare professionals who will be working in a critical care role that is different to their current role and require some additional critical care training to enable them to do the job.
Pink education and training for those who will be working in a critical care unit in a role that is significantly different to their current practice. These roles are healthcare support roles, may have direct patient responsibility but will be part of care teams overseen by a registered healthcare practitioner.
These scenarios were written to support the face-to-face training within the Yorkshire & Humber Nightingale Education team.
Step Three: Sharing your resources and feedback
The skills matrix and educational resources are still being developed and we would appreciate any feedback and contribution you may have to support their finalisation. You can contact us on LTLC@hee.nhs.uk. See the drop-down sections below for more information.
-
Skills matrix
There are 2 ways to give feedback on the skills matrix:
A. Use this survey link below to provide us with some feedback on the skills matrix. This resource is under constant review so your input is highly valued. The survey is designed for both learners and educators and should take no longer than a few minutes to complete. Thank you in advance for completing it.
B. For more detailed and specific feedback you can download a copy of the ‘Skills matrix Excel’, and make direct edits to email to us. We would appreciate input on the following areas:
- A change to language – please add “notes” on the excel with the appropriate language and rationale, and indicate in your email body the areas you have made recommendations on
- Addition or deletion of a skill – please add new rows to the excel and put additions in GREEN, or highlight suggested deletion skills in RED
- Essential vs desirable – please indicate this by writing in column D (in a contrasting colour or highlighting a cell where a change has been made)
- Educational resource recommendations – please see the below section on ‘Educational resources’
- An indication of how you intend to use the skills matrix – we would be interested for feedback on the usability of the skills matrix. If making suggestions, please provide enough of an explanation that your input can be actioned
- Links to other competency frameworks – please provide links to (or copies of) competency frameworks which should inform this skills matrix
-
Educational resources
The LTLC are collating existing high-quality education resources developed across London to make them openly accessible. We are asking anyone with such a resource to send it to LTLC@hee.nhs.uk. If you are able to complete the attached coversheet (Microsoft Excel, 15KB) we would be grateful but this is not imperative as we really need any resources submitted ASAP.
Please ensure that you have permission from those involved in its development before you share it with us. When sharing the resource, we will always attribute authorship to the original authors. We may make minor edits before it is shared to ensure that the content is accurate, up-to-date and in a standardised format. Please note that LTLC are not responsible for the resource after it has been shared.
The resources we are looking for include any critical care related educational resource from all professions, such as:
- Lesson plans
- ICU competency frameworks (especially occupational therapists, physiotherapists, SALT, dieticians, pharmacists)
- Video content
- Simulation scenarios
- PowerPoint lectures
Examples of topics we are interested in are:
- ICU skills such as ventilation, ICU drugs, tracheostomy management etc
- Profession specific topics (for example, content developed by dieticians to teach ICU feeding)
- ICU rehabilitation and delirium
- Moving and handling intubated patients
- Equipment training, such as ventilators and infusion pumps
- ICU leadership
- Wellbeing
- Up-to-date COVID management
Managing the COVID Surge: 10 Quick Wins for ICUs
Frontline clinicians working with the National CLEAR Programme for ICU, as part of the LTLC, are sharing ten recommendations that can be adopted in ICU in 48 hours. While working collaboratively across four London trusts, clinicians identified these “quick wins” in response to the experience and reflections of staff in the first wave of the pandemic.
-
Managing the COVID surge: 10 Quick Wins for ICUs
Managing the COVID surge: 10 Quick Wins for ICUs
The National CLEAR Programme provides training, data analytics and modelling tools for Clinically-Led workforcE and Activity Redesign (CLEAR). CLEAR participants working in ICUs across 4 London trusts have identified ‘quick wins’ to share with colleagues across the NHS. Whilst these recommendations may seem straightforward and ‘common sense’, our evidence shows that they improve communication, staff wellbeing and patient care.
All of the recommendations can be adopted within 48 hours. The 10 Quick Wins infographic (PDF, 1125KB) provides a summary checklist for discussion in multi-disciplinary planning forums and staff meetings. Download the printer ready version (PDF, 295KB). The 10 Quick Wins slidedeck (PDF, 820KB) provides further details and practical examples.
Research outputs informing our programme
-
Learning from the Education Experiences of ICU Staff (Survey)
The LTLC have surveyed almost 1000 ICU staff from across London in order to understand their experiences of education during the COVID pandemic. This includes critical care educators, critical care staff who received education and staff redeployed to ICU. The feedback that has been received from across London is informing the work of the LTLC, including the co-development of the skills matrix and the collation of resources.
Summary of results
Please find below summaries of the survey results broken down by group:
- ITU staff who primarily delivered education (PDF, 790KB)
- ITU staff who primarily received education (PDF, 391KB)
- Redeployed nursing staff (PDF, 1061KB)
- Redeployed occupational therapists (PDF, 794KB)
- Redeployed speech and language therapists (Microsoft PowerPoint, 428KB)
- Redeployed Dieticians (PDF, 1490KB)
- Redeployed Physiotherapists (PDF, 1174KB)
- Redeployed Doctors (Microsoft PowerPoint, 445KB)
- Healthcare Assistants (PDF, 1454KB)
- Redeployed healthcare scientists (Microsoft PowerPoint, 423KB)
- Redeployed Pharmacists (Microsoft PowerPoint, 406KB)
- Other redeployed staff groups (PDF, 1232KB) including operating department practitioners dentists/dental assistants and nurses, students, podiatrists, midwifes, nursing associates and advanced clinical practitioners
-
A Survey into the Workforce utilised to Support Critical Care Units during COVID-19
Two short surveys were developed in collaboration between the Intensive Care Society (ICS) and the Operational Delivery Network (ODN) representatives, and disseminated via Survey Monkey over the month of May 2020. One was specifically for critical care managers/nurse leads to complete, the other for staff who were redeployed into critical care.
The aims of the surveys were to obtain a snapshot of the additional workforce mobilised to manage critical care surge during the COVID-19 crisis. The aim was that that the data returned can help inform areas of good practice, and identify areas for improvement in future, should the need for staff redeployment to critical care be required again.
Download the results of the survey (PDF, 885KB).
-
LTLC Emerging Findings: Changes to Models of Care on ICU (infographic)
Results from a rapid qualitative appraisal based on telephone interviews with staff across ICUs in London to:
- document changes made it ICU models of care
- explore challenges and enablers in the implementation of these changes
- identify the aspects of care delivery that worked well and areas for improvement
Download the infographic (PDF, 6460KB).
-
NHS Staff Experiences of Working in Critical Care – The CLAP Study (infographic)
Results of telephone interviews with 40 staff from critical care units in Scotland and England.
Download the infographic (PDF, 1527KB).
Additional materials
-
FICM and HEE Skills Passport
“The entire intensive care community is keen to acknowledge the contributions made during the COVID-19 pandemic by many members of the multidisciplinary team (MDT). In particular, those who were deployed into Critical Care areas, joined rotas, used existing skills, and cross-skilled as abilities and supervision permitted.
The Faculty understands that for medical trainees, nurses and Allied Health Professionals (AHPs) who do not generally work in Critical Care, getting recognition for any new or added ICM skills obtained during the pandemic can be problematic. In conjunction with Health Education England (HEE), we have developed a ‘COVID Passport’ to help those individuals get the recognition they deserve.
The Passport is comprised of two sections:
- Care Packs: Each ‘Care Pack’ contains examples of skills and work undertaken during deployment to Critical Care that individuals can denote that they have completed. This section is counter-signed by a supervisor in ICM (this may be a consultant, charge nurse, senior AHP or line manager, as appropriate) to certify that the health professional has worked in these general areas to the denoted level of supervision.
- Skills Self-Certification: Specific skills developed can be delineated further, in the ‘COVID-19 Skills Passport Clarification’ section of the document. This will provide future employers and trainers with more detail on individual attainments. Please note that this section is entirely self-certified and is not signed-off by an ICM supervisor.”
-
Delivering oxygen therapies
This resource (PDF, 6.6MB) was designed as a high-level document to highlight the risks of a catastrophic event relating to oxygen use, limited supplies and failure. The following topics are covered:
- Catastrophic oxygen failure and mitigating the risks
- Oxygen consumption and good housekeeping guidance
- Risk of fire and mitigating actions
This resource is designed for all clinical staff working in areas delivering oxygen therapies. This document does not present any original guidance; national and regional guidance has been collated where appropriate. All guidelines used are referenced and linked in the relevant sections. This document is correct at the time of construction (January 2021); however, please be aware that specific guidelines may change with time.
Further information
NHS England/Improvement and Health Education England have worked in partnership to develop this approach which has already been extensively tested with stakeholders.
Please contact the LTLC team for any further information or questions about the programme (ltlc@hee.nhs.uk)
How to access
The London Transformation and Learning Collaborative (LTLC) programme, you will need an elfh account. If you do not have one, then you can register by selecting the Register button below.
To view the London Transformation and Learning Collaborative (LTLC) programme, select the View button below. If you already have an account with elfh, you will also be able to login and enrol on the programme from the View button.
Registering large numbers of users
If you are a HR, IT or Practice Manager and would like to register and enrol large numbers of staff within your organisation for access onto the London Transformation and Learning Collaborative (LTLC) programme, please contact elfh directly.
More information
Please select the following link for more information on how to use the elfh Hub.